Addressing Public Health Determinants Through Community Benefits at CleanMed and Beyond
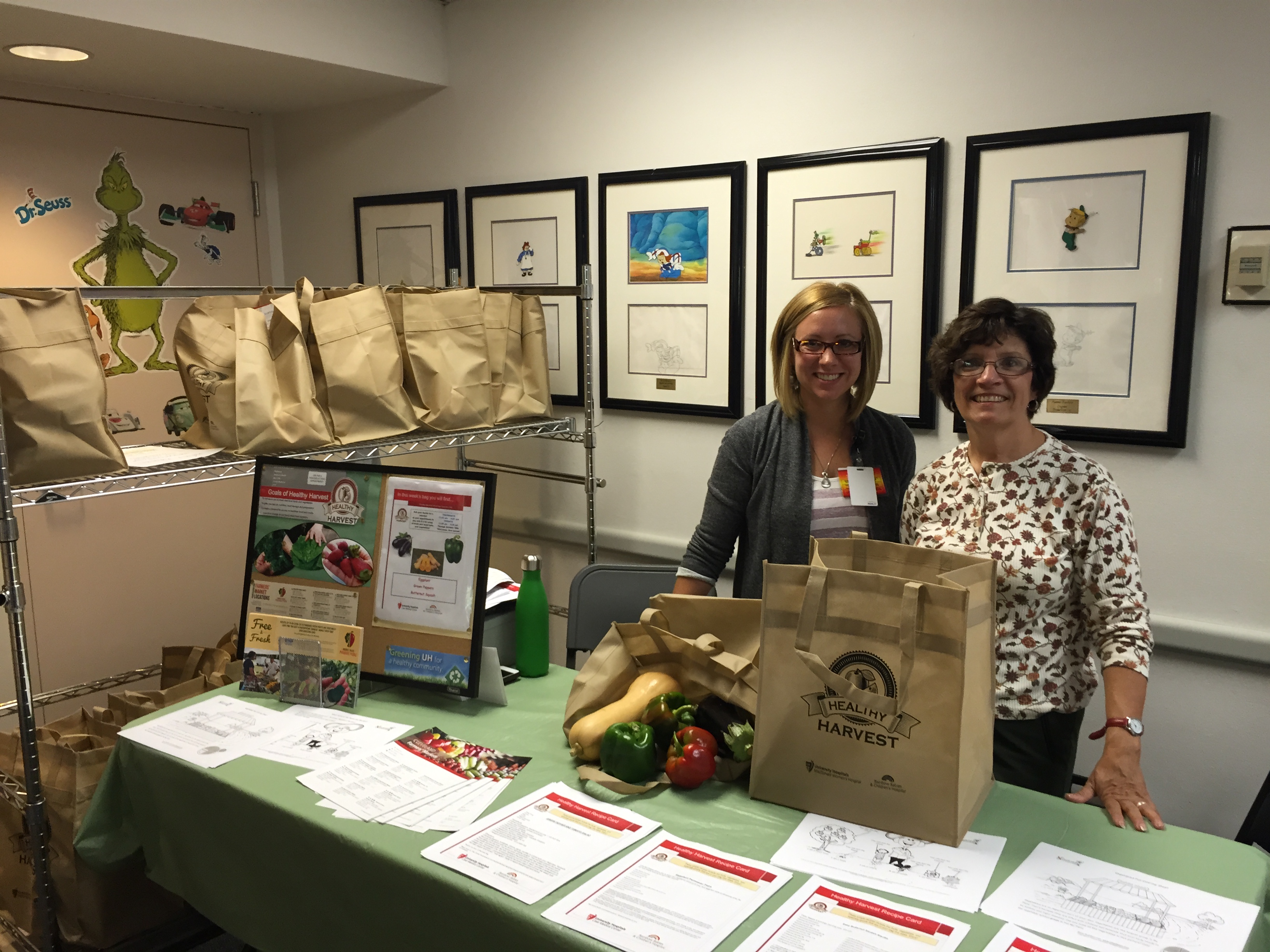
The Healthy Harvest program at University Hospital, Rainbow Babies Clinic in Cleveland, OH provides bags of fresh, local produce to low-income moms in their clinic with support from their Community Benefits program (Matt Pietro).
There is a powerful new opportunity for nonprofit hospitals to collaborate with other stakeholders to implement community health improvement plans that address social determinants of health such as housing, environmental and safety conditions, and the availability of quality, affordable food.
The IRS recently changed the rules regulating the ways nonprofit healthcare facilities can address public health issues through their community benefit obligations. These changes represent an important shift in focus for the U.S. healthcare community—from treating sickness and disease to promoting prevention and wellness.
The IRS rule outlines that “the need to prevent illness, to ensure adequate nutrition, or to address social, behavioral, and environmental factors that influence health in the community,” can be used to define and inform community benefits work.
In addition, 2014 updates to the Affordable Care Act (ACA) require nonprofit hospitals to conduct community health needs assessments every three years, and develop an implementation plan to address these challenges.
While almost three quarters of community benefit funds are used to help pay for care for the uninsured or underinsured, funding for community health improvement and community building activities represented approximately 5% of community benefit activities according to a 2009 Ernst & Young report.
The new rule could be especially effective for addressing nutritional deficiencies and diet-related health issues. Over 48 million Americans are food insecure, defined by the USDA as “as lack of access to “enough food for an active, healthy life.” At nearly $190 billion per year, annual expenses associated with obesity (and diet-related diseases) now exceed the cost of smoking as a public health threat.
These changes pave the way for the health sector to invest in a wide spectrum of nutrition-related programming from acute food insecurity interventions to long-term efforts in building vibrant regional food systems by supporting local growers and economies.
Healthy Food in Health Care (HFHC), a program of HCWH has begun to investigate the ways in which hospitals are utilizing their community benefit programs to identify and support interventions for diet-related health conditions in their communities, and opportunities for expanding this role.
“Since most of our communities are plagued by diet related diseases—obesity, diabetes, and heart disease—it only makes sense for facilities to be addressing the root causes of these diseases. One of the most effective ways they can do this is by investing in the community food environment to make healthy food the easy choice regardless of zip code.” -Dr. Jennifer Obadia, the New England Coordinator for the Healthy Food in Health Care at Health Care Without Harm.
In a three-year project, funded by the Robert Wood Johnson Foundation, HCWH will undertake a national study of nonprofit hospitals’ community benefit practices targeted at strengthening food system resilience and sustainability, improving physical and economic access to healthy foods, and promoting healthier dietary patterns and healthy body weight.
“I’m excited to see the new forms of hospital community health engagement with food environments that is emerging throughout the country. Through this study, we will identify best practices and model programs. We will also collaborate with other stakeholders to disseminate tools and resources to promote healthier, more sustainable, and more equitable food systems.” - Susan Bridle-Fitzpatrick, PhD Senior Researcher, Healthy Food in Health Care
This year at CleanMed, the premier national environmental conference for leaders in healthcare sustainability, several experts in the field of community benefits including Ellen Tohn, Dr. Jennifer Obadia, Pamela Schwartz and Susan Bridle-Fitzpatrick, Phd, will be discussing the changes to the community benefit standard and the opportunities that exist to address costly diet-related diseases diseases such as diabetes and obesity through a prevention based environmental health approach.
This session is part of a larger discussion at CleanMed in which health professionals are exploring ways to bring a climate change lense to community health needs assessments and to adopt strategies that address immediate needs with longer term climate change co-benefits.
Register today for CleanMed and you can look forward to this and many other sessions focused on sustainable, healthy food in health care.
Learn more about identifying local health priorities and expanding community benefit initiatives in the 2016 Health Care Without Harm report, Leveraging Hospital Community Benefit Activities to Address Climate Change and Environmental Risks.
